Women’s Health Services and Treatments
We specialize in the many women health issues that can affect women throughout their lifecycles, from puberty to menopause. If you experience any of the following symptoms, we can help you:
- Leaking urine when coughing, sneezing or laughing
- Low back pain or pelvic pain during pregnancy
- Hesitation to laugh heartily in case of pant wetting
- Stopping running because of unpleasant wetness
- Pelvic Girdle Pain during pregnancy
- Visiting the bathroom more frequently than normal
- Not always able to hold on until reaching bathroom
- Pain in the pelvic area
- Unable to put off the urge to pee
- Constipation
- Sex is uncomfortable
Physiotherapy treatment is always carried out in a private treatment room, always with the same Physiotherapist, providing sensitive, professional treatment. It starts with a thorough assessment. Detailed questions will ask about your pain, affects on your lifestyle, your medical history, questions about your bladder, bowels, diet and menstrual cycle. A physical examination will then follow, which may include your posture, lower back, hips and abdominal muscles and an internal vaginal and/or rectal examination.
Once the examination is complete, a discussion follows, explaining the findings, and exploring treatment options. It is a good opportunity for you to ask questions to gain a better understanding of your problems.
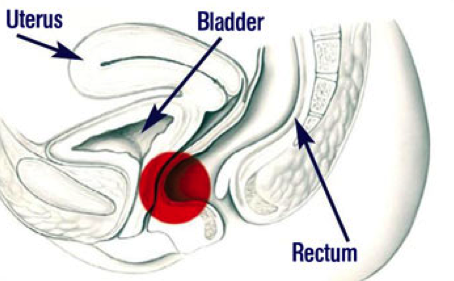
Bladder Problems – Urinary Incontinence
Technically not perfect but illustrative, the pelvic floor can be compared to a hammock. Bladder, rectum and, with women, the uterus are kept in their intended position by this hammock. In the course of life, this construction of muscles and connective tissue is often additionally exposed to enormous strains. This includes, among other things, permanent hard physical labour, as well as pregnancy and birth. Issues such as a low-fibre diet without sufficient supply of liquids, and obesity, can also strain the pelvic floor. The unawareness of one's pelvic floor also plays an essential role here. Weak pelvic floor muscles (hypotonicity) contributes to stress incontinence, urge incontinence and pelvic organ prolapse.
Urinary incontinence is the unwanted loss of urine at the wrong time or the wrong place. It can be just a few drops or enough to run down your legs.
There are many myths surrounding urinary incontinence, such as it’s an inevitable part of aging, or to be expected after childbirth. However, urinary incontinence can affect anyone of any age, of either sex. It’s estimated to affect 1 in 4 women at some point in their lives, 1 in 10 men and 1 in 5 seniors.
Stress Incontinence is the most common type of urinary incontinence. It is a loss of small to moderate amounts of urine with exertion, like coughing, sneezing, jumping, running, laughing, changing position, etc. Often this is due to weakness of the pelvic floor muscles, in women this can be following childbirth or the menopause, with men, it is a common problem after prostate surgery.
Urge Incontinence is a loss of urine (sometimes large amounts) following an urgent need to empty the bladder. The urge can be extremely strong and impossible to ignore. People suffering from urge incontinence often need to go to the washroom very frequently during the day and sometimes frequently at night too. They will typically plan their days around finding the next washroom.
Mixed Incontinence is a combination of stress and urge incontinence.


Physiotherapy Treatment for Incontinence
Treatment is focused around the pelvis floor muscles, the sling of muscles that help to support and control the bladder. You will be taught how to identify them, how to tighten them (Kegel exercises), and how to use them functionally to keep you dry (‘the Knack’). Computerised Biofeedback is a very useful tool in teaching pelvic floor muscle awareness and strengthening. Through the use of carefully placed electrodes you are able to see on a computer screen the affect of tightening your pelvic floor muscles.
Being able to see when the muscles are working effectively teaches you how to control muscles that you may previously have been unaware of.
Other techniques may include bladder retraining, posture reeducation, exercises for the abdominal and other core muscles.
A home exercise programme will always be an important part of your treatment.
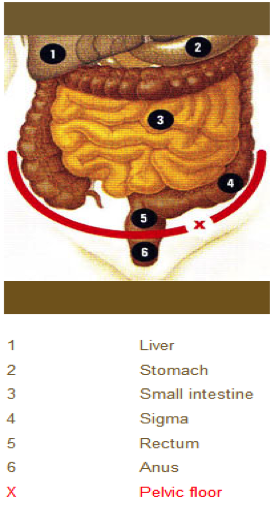
Bowel Problems
Fecal incontinence is the loss of bowel control resulting in a loss of gas, liquid or solid stool. It can affect men and women of any age.
Symptoms can range from being unable to control the passing of gas or losing small ‘pellets’ without being aware of the loss, to having an extreme urge to get to the washroom and not making it in time.
Whatever the problem, the embarrassment and anxiety it can create can severely affect your confidence, with the fear of repeated accidents always in the back of your mind.
There can be many different causes of bowel leakage. The most common cause is weakness of, or damage to, the rings of muscle that circle the anus. These are called the external and internal anal sphincter muscles and they sit just below the pelvic floor muscles.
The external anal sphincter works to delay a bowel movement if an urge is felt but it’s not convenient to go to the washroom right away. If it is weak, you will have an urgent need to get to the washroom immediately, and may lose some bowel contents if you can’t get there in time.
Either one, or both of these muscles can be damaged. The most likely cause of damage is childbirth, when the muscles may easily be stretched or torn. If there is a tear at the back of the vagina (often called a 3rd or 4th degree tear) when forceps are used or the baby is very large, damage is more likely to have occurred.
You may be aware of difficulty controlling your bowels immediately after the birth, or problems may develop many years later, as the pelvic floor muscles (which also help with bowel control) and sphincter muscles gradually weaken with age or recurrent straining.
The muscles may also be damaged during surgery to the rectum or anus, and may be weakened by years of straining to empty the bowels.
Constipation is where it is difficult to pass a motion due to imbalance of the pelvic floor muscles. The patient might have an inability to coordinate the abdominal, pelvic floor and sphincter muscles together, in order to evacuate stools without straining. Chronic constipation is frequently a cause of stretching and weakening of the pelvic floor muscles.
Physiotherapy Treatment for Bowel Problems
The goal of our physiotherapy treatment for bowel problems is to teach you to regain control of your bowels. Treatment will always involve a lot of education, to teach you simple measures that can make a big impact on your bowel control.
Treatment may focus on various groups of muscles that are involved in maintaining bowel control; the pelvic floor muscles, the abdominal muscles and the anal sphincter muscles. The muscles may need to be strengthened, and taught to work together in a coordinated way, or taught how to relax. Biofeedback may be used as a tool to improve muscle and bowel awareness.
Because you cannot see the pelvic floor muscles, you may have found it difficult to locate them. Perhaps you are uncertain if you are doing the pelvic muscle exercises correctly. This is where biofeedback can help. With the use of internal electrode biofeedback therapy uses computer graphs and audible tones to show you the pelvic floor muscles you are contracting or relaxing. It also allows the therapist to measure your muscle strength and individualize your exercise program. It does not do anything to your muscles. It is a teaching tool to help you learn to control and strengthen the pelvic floor muscles more effectively.
Treatment may also look at food and drink intake, techniques to avoid straining when passing a bowel movement, and look at overall posture and muscle support. A home exercise program will always be an important part of your treatment.
Frequently, there may be a combination of bowel and bladder problems. Both can be helped with treatment.
Throughout treatment you will be given support and encouragement as you begin to learn and use new techniques to gain control of your bowels.
Chronic Pelvic Pain
Chronic pelvic pain is a common problem, affecting many women. It is pain that may be felt in and around the genitals, the rectum, pelvis, groin, abdomen, hips, thighs or buttocks. It may be mild or severe, constant or only on certain activities such as vaginal insertion, exercising, cycling, sitting or wearing certain clothing. The pain may be described as burning, aching, stabbing, shooting, or like ‘paper cuts’ or ‘something ripping’.
The pain may have been present for many years, seemingly without a reason, or may have started following a trauma to the pelvic floor during childbirth, injury to sacrum or coccyx (falls), chronic constipation or due to tight overactive pelvic floor muscles (hypertonicity).
Hypertonic pelvic floor muscles contribute to urinary urgency, urge incontinence, constipation and any of following conditions, all of which we treat:
- Pelvic floor/perineal pain
- Vaginal/rectal pain
- Lower abdominal pain
- Vulvodynia
- Coccydynia
- Vaginismus
- Levator Ani Syndrome.

Physiotherapy Treatment For Chronic Pelvic Pain
Physiotherapy treatment for chronic pelvic pain is focused on the pelvic floor muscles, teaching you to be able to identify them, how to tighten and relax them and reduce the tension in them. It is the ability to relax the pelvic floor muscles that provides the key to breaking the pain, i.e. PF muscle spasm leading to the pain cycle.
This muscle spasm is similar to the spasm and tension people often get in the neck and shoulder muscles, but in that case you are often aware of the tension and you can feel your muscles tightening, and see the effect as your shoulders rise up towards your ears. You can use techniques to reduce the tension, such as massage, exercises and relaxation techniques, or just remind yourself to let go of the muscles. However, with the pelvic floor muscles we are often unaware that they exist, let alone aware that they might be in spasm or particularly tight. If we are unaware of the muscles, then we are unlikely to be able to relax them or reduce the tension in them.
Computerized biofeedback is a very useful tool in teaching pelvic floor awareness and relaxation. Through the use of carefully placed electrodes or internal electrodes, you are able to see on the computer screen the activity of your pelvic floor muscles. Being able to see when the muscles are contracting and when they are relaxed teaches you how to control muscles that you have previously been unaware of.
Muscles which have been in spasm for a long period of time will often become shortened and tight (hypertonicity). Manual therapy or ‘hands-on’ techniques, including internal and external triggerpoint therapy (releasing muscle knots), can be used to treat the painful muscles and gradually stretch the muscles and tissues to improve their flexibility. Work can then be done to strengthen them. This might involve the muscles of the pelvic floor, hips, buttocks, back or abdominal area.
If an internal examination is too painful, the connective tissue of your abdomen, thighs, groins and lower back are often very tight. The connective tissue forms the container of the muscles and this tissue often needs to be relaxed before any internal work can be done.
Throughout treatment you are given support and encouragement, as self-care is an important part of the treatment. Avoid straining and pushing during toilet visits, you begin home exercise program with breathing exercises and learn techniques to take control of your symptoms.
Persistent pain education is an important part of treating pelvic floor dysfunction, since the pelvic area is an area that we often hold our stress. Anxiety, stress and our thoughts, attitudes and beliefs can perpetuate the pain in our pelvis. Understanding how our pain works has shown to be an effective way of reducing the threat of ongoing pelvic pain.
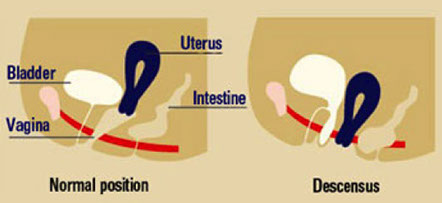
Prolapse
Pelvic organ prolapse is a common condition, particularly affecting older women. Prolapse literally means ‘to fall’ and it occurs when the structures designed to keep organs in place weaken or stretch so that one or more pelvic organs (the uterus, bladder, bowel or rectum) starts to slip out of place.
It is the pelvic floor muscles and supporting ligaments that keep the pelvic organs in their proper position. The pelvic floor muscles may become weakened for many reasons, such as pregnancy and childbirth, ageing, heavy lifting, obesity, chronic straining, surgery or injury.
The type of prolapse you have is named according to which structure has slipped. These are the most common types:
- Cystocele (bladder prolapse): the bladder drops down and bulges into the front wall of the vagina.
- Rectocele (prolapse of the rectum): the rectum bulges into the back wall of the vagina.
- Uterine Prolapse (prolapse of the uterus): the uterus (womb) drops down into the vagina. In severe cases it can drop below the vaginal entrance, to sit outside the body.
As with many conditions, the prolapse may be mild, moderate or severe and many women with a mild prolapse will be unaware of it, and may not experience any problems from it. Other women will be aware of a bulging sensation in the vagina, particularly at the end of the day, or after doing a lot of lifting or repeated coughing.
Problems women may have as a result of a prolapse can vary as follows:
- A sense of ‘something coming down’ or a ‘dragging feeling’
- Seeing or feeling a lump in the vagina
- Bladder problems like stress, urge or overflow urinary incontinence (see bladder problems)
- Difficulty emptying the bowels
- Lower back or pelvic pain
- Pain or discomfort during sexual intercourse
Physiotherapy Treatment for Pelvic Organ Prolapse
Physiotherapy will not be able to return the prolapsed pelvic organ(s) to their original position, but it can help improve the strength of the pelvic floor muscles so that they provide more support to the pelvic organs and prevent further slippage.
Physiotherapy can also play an important part in teaching you how to avoid certain activities and help you make simple lifestyle changes which will prevent you from causing further damage to, and stretching of, your pelvic floor muscles. It can also teach you how to improve your bladder control.
The physiotherapy goal is to reduce the symptoms caused by the prolapse and to improve your pelvic floor support. Treatment will always involve a lot of education, to teach you simple measures that can make a big impact on your comfort and control, for instance instructions on how to pass bowel movements without straining.
Treatment is often focused around the pelvic floor muscles – the sling of muscles that help to support and control the bladder. You will be taught how to identify them, how to tighten them (Kegel exercises) and how to use them functionally to help support your pelvic organs during daily activities.
Treatment techniques may include computerized biofeedback, to teach pelvic floor muscle awareness, bladder retraining and posture reeducation. A home exercise program will always be an important part of your treatment.
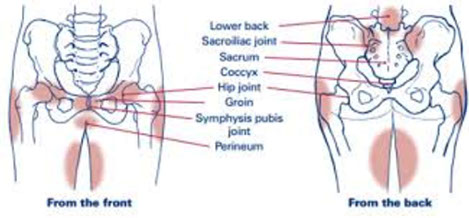
Pelvic Girdle Pain
Pelvic Girdle Pain (PGP) was formerly known as Symphysis Pubis Dysfunction (SPD).
There is a wide range of symptoms and the severity varies between women. The main symptoms are pain while walking, climbing stairs and turning over in bed.
This means that it affects virtually everything you do in a day and can have a major impact on your life. Pain can be at the front and/or back of your pelvis at any stage during or after pregnancy. PGP is treatable at any stage of pregnancy or postnatally, as soon as you feel able to visit your therapist.
Physiotherapy Treatment for Pelvic Girdle Pain
The aim of treatment is to assess the position and the symmetry of movement of your pelvic joints, especially the sacroiliac joints at the back of the pelvis.
Treatment involves a combination of joint mobilisation and soft tissue or muscle treatment. This is because the muscles often become tight or over compensate when you have a lot of pain.
This tightness has to be released to allow the joint to move normally and prevent the problem from happening again, as soon as you leave the therapist’s room. Gentle hands-on techniques are used and gentle exercises will be given to help your pelvic stability. As you recover, your exercise programme will be adapted to suit your individual needs, until you get back to normal.
Biofeedback Treatment
Biofeedback takes information about something happening in the body, and presents it in a way that you can see or hear, and understand. Getting on a scale to check your weight or having your blood pressure taken are very simple examples of biofeedback. These can be used to measure any body response, such as heart rate or muscle contraction and relaxation. We use biofeedback mainly with our bladder and bowel patients, and in patients with jaw pain.
In biofeedback the measurement can be displayed on a computer screen, or heard as a tone, and used then to learn about a subtle body function.
Biofeedback treatment for Bladder and Bowel problems
The Pelvic Floor Muscles (PFM) are a group of muscles that play an important role in bladder and bowel control. Weakness or dysfunction of the pelvic floor muscles can lead to problems with both bladder and rectal support and control.
Biofeedback has been proven effective in the treatment of urinary incontinence in numerous research studies. It is also used in patients with fecal incontinence and in teaching patients with over active PFM to relax the muscles. It can be used to help learn to control and strengthen/or relax the PFM.
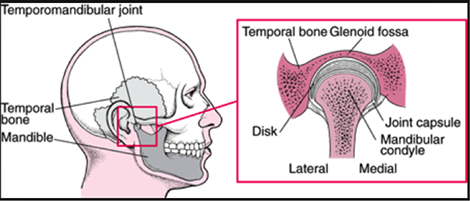
Biofeedback treatment for jaw pain or TMJ Dysfunction
Your Temporomandibular Joint (TMJ), or jaw joint, is the most used joint in the body. Your TMJs are involved with eating, talking, breathing and, probably most importantly, expressing our feelings and emotions. When things go wrong with your TMJ, it is known as Temporomandibular Disorder (TMD).
In our clinics we have a keen interest in treating patients with TMJ problems. Mark wrote his thesis in his 4th Year of college on ‘Physiotherapy and TMJ Dysfunction’. Cynthia has many years experience in treating TMJ problems with EMG biofeedback.
TMJ Symptoms
You may or may not experience jaw pain or tenderness with TMJ dysfunction. The most common symptoms include:
- Clicking
- Popping
- Grinding
- Limited opening
- An inability to fully clench your jaw
TMD sufferers are often teeth grinders or clenchers. They can also suffer headaches, ear pain dizziness, and upper neck pain. Some TMJ patients report pain or inability to eat, talk or sing. Tinnitus or ear ringing can be associated with TMJ dysfunction.