Men’s Health Services and Treatments
Men’s health involves conditions that affect men throughout their lifespan from childhood through adulthood. Men can experience musculoskeletal injuries, such as back, neck and pelvic pain, from daily activity or sports. Men can also experience bladder and bowel disorders, including urinary urgency/frequency/incontinence, constipation and hemorrhoids.
Pelvic floor physiotherapy can be extremely helpful in addressing some of the challenges that men have when their pelvic floor muscles are not working properly, including:
- Post-prostatectomy urinary incontinence
- Chronic Pelvic pain including testicular and penile pain and chronic prostatitis
- Chronic constipation
- Tight pelvic Floor muscles
- Erectile dysfunction
Urinary Incontinence can have many causes and understanding your symptoms is easier if you understand how the normal bladder works.
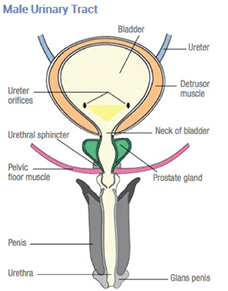
The bladder is the sac where urine is stored. It’s the size and shape of a grapefruit and can hold about 300–500ml of fluid. Urine is filtered by the kidneys and drains into the bladder through two tubes called ureters. From the bladder, urine leaves the body through the urethra. Together, this group of organs and tubes is called the urinary tract.
The wall of the bladder is made of several layers. The thickest of these layers is called the detrusor muscle. As the bladder fills up, the bladder wall expands. When it’s time to urinate, the detrusor muscle contracts to push the urine out.
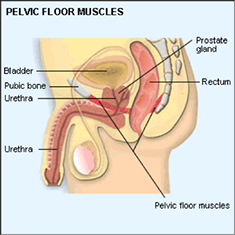
A man’s pelvic floor muscles support his bladder and bowel. The urine tube or urethra and the back passage pass through the pelvic floor muscles. The pelvic floor muscles help to control your bladder and bowel. It is vital to keep your pelvic floor muscles strong and healthy.

Physiotherapy Treatment for Urinary Incontinence Post Prostatectomy and TURP
Bladder problems are a common side effect of prostate surgery. Most men regain their bladder control over time and are fully recovered within 6-12 months, however pelvic floor muscle exercises are key to this. Increased pelvic floor muscle strength and fitness can speed up a man’s bladder control following radical prostatectomy and transurethral resection of the prostate (TURP).
Performing pelvic floor muscle exercises after prostate surgery is vital to your recovery as it these muscles that help to control your bladder. Physiotherapy treatment will include:
- Evaluate current function, muscle strength testing including pelvic floor.
- P.F. Muscle re-education utilizing biofeedback.
- Bladder re-education.
- Postural education.

Chronic Pelvic pain
Pelvic pain encompasses several conditions that cause pain throughout the pelvis and can also cause difficulty with bladder frequency and urgency, bowel (constipation) and sexual function.
Pain, pressure or ache can be felt in the tailbone, rectum, or pelvic (testicular and penal pain). The symptoms may be intensified by prolonged sitting, sexual activity, defecation and constipation. The pain can refer or travel to the legs, tailbone or buttocks. Severe sharp burning or aching during urination may also occur. This can be caused by unusual tension in the levator ani or pelvic floor muscles.
Pain can be arising from the prostate gland (chronic prostatitis/chronic pelvic pain CP/CPP).
Many studies have shown that men with chronic pelvic pain have very little inflammation (as measured by white blood cells, or pus cells, in their prostatic fluid).
It is estimated that pelvic floor muscle spasm may be the main cause of symptoms in the majority of chronic pelvis pain/chronic prostatitis patients. It is recommended that everyone with CP/CPP should have a pelvic floor examination, as part of a complete urological work-up by physiotherapist specialist in trigger point/myofascial evaluation.
Physiotherapy Treatment For Chronic Pelvic Pain
Physiotherapy treatment is focused on the pelvic floor muscles, teaching you to be able to identify them, how to tighten them and, therefore, how to relax them and reduce the tension in them. It is the ability to relax the pelvic floor muscles that provides the key to breaking the pain → muscle spasm → pain cycle.
This muscle spasm is similar to spasm and tension people often get in the neck and shoulder muscles, but in that case, you are often aware of the tension, you can feel your muscles tightening and see the effect as your shoulders rise up towards your ears. You can then use techniques to reduce the tension, such as massage, exercises, relaxation techniques, or just remind yourself to let go of the muscles. However with the pelvic floor muscles, we are often unaware that they exist, let alone aware that they might be in spasm or particularly tight. If we are unaware of the muscles, then we are unlikely to be able to relax them or reduce the tension in them.
Computerized biofeedback is a very useful tool in teaching pelvic floor awareness and relaxation. Through the use of carefully placed electrodes or internal electrodes, you are able to see on the computer screen the activity of your pelvic floor muscles. Being able to see when the muscles are contracting and when they are relaxed, teaches you how to control muscles that you have previously been unaware of.
Muscles that have been in spasm for a long period of time will often become shortened and tight (hypertonicity). Manual therapy or ‘ hands-on’ techniques including internal and external triggerpoint therapy (releasing muscle knots) can be used to treat the painful muscles and gradually stretch the muscles and tissues to improve their flexibility. Work might then be done to strengthen them. This might involve the muscles of the pelvic floor, hips, buttocks, back or abdominals.
If an internal examination is too painful, the connective tissue of your abdomen, thighs, groins and lower back are often very tight. The connective tissue forms the container of the muscles and this tissue often needs to be relaxed before any internal work can be done.
Throughout treatment you are given support and encouragement, as self-care is an important part of the treatment. Avoid straining and pushing during toilet visits, you begin a home exercise program with breathing exercises, and learn techniques to take control of your symptoms.
Persistent pain education is an important part of treating pelvic floor dysfunction since the pelvic area is an area that we often hold our stress. Psychosocial factors such as anxiety, stress and our thoughts, attitudes and beliefs can perpetuate the pain in our pelvis, understanding how our pain works has shown to be an effective way of reducing the threat of ongoing pelvic pain.
Constipation
Chronic constipation is frequently a cause of damage to the pelvic floor muscles and fascial support (ligaments). Chronic constipation can cause stretching of the pudendal nerve due to prolonged and repetitive straining (leading to pelvic floor weakness secondary to nerve damage).
Constipation also creates more pressure on the bladder and urethra, which may cause increased urinary frequency or retention.
When you are constipated, general recommendations on diet (fluid and fibre intake), toilet habits and positions, breathing/pelvic floor relaxation exercises and bowel mobility exercises such as the abdominal massage, all need to be considered.
Your ability to consciously relax your pelvic floor muscles is a critical part of your recovery program. You must learn to relax these muscles before they can become functional again. The feeling of dropping your pelvic floor is similar to the moment of relief when you have reached the bathroom. When you urinate or have a bowel movement, you first drop your pelvic floor and let the pelvic floor muscles (PFM) go. Pay attention to this and see if you can feel that happening. The key to dropping your pelvic floor is visualization and deep breathing. The best way to consciously release tension from the PFM’s is to try to release the muscles while you inhale.
When you relax your pelvic floor muscles, it should also feel like you are creating more space between the pubic bone and tailbone. Don’t make it happen, visualize and let it happen!
Eventually, once we have taught you ’the art ‘of relaxing your pelvic floor muscles, you will need to check in with your pelvic floor throughout the day, and let go of any tension that you discover. Together with correct defecation posture and techniques we will work up to an easier bowel emptying, without straining.
Physiotherapy for Constipation
When you are constipated, general recommendations , diet (fluid and fibre intake), toilet habits and positions, and breathing /pelvic floor relaxation exercises and bowel mobility exercises such as the abdominal massage all need to be considered.
Your ability to consciously relax your pelvic floor muscles is a critical part of your recovery program. You must learn to relax these muscles before they can become functional again. The feeling of dropping your pelvic floor is similar to the moment of relief when you have reached the bathroom; when you urinate or have a bowel movement, you first drop your pelvic floor, and let the pelvic floor muscles (PFM) go. Pay attention to this, and see if you can feel that happening. The key to dropping your pelvic floor is visulasation, and deep breathing. The best way to consciously release tension from the PFM’s is to try to release the muscles while you inhale.
When you relax your pelvic floor muscles, it should also feel like you are creating more space between the pubic bone and tailbone. Don’t make it happen, visualize and let it happen!
Eventually, once we have taught you ’the art ‘of relaxing your pelvic floor muscles, you will need to check in with your pelvic floor throughout the day, and let go of any tension that you discover. Together with correct defecation posture and techniques we will work up to a easier bowel emptying with no straining.